A process that normally takes years to develop and move vaccines through clinical testing and approval has been fast-tracked to just months. Pfizer/BioNTech won the initial race, with Oxford University/AstraZeneca and Moderna’s vaccines coming in closely behind them.
Although it has been an incredible feat of scientific development to produce these vaccines so quickly, they do not come without challenges.
Two of the three vaccines must be shipped and stored at a temperature between –4 °F (Moderna) and –94 °F (Pfizer/BioNTech) and can only be kept thawed in a fridge for a limited time before the lipids degrade.1
And whereas the Oxford University and AstraZeneca vaccine is easy to store and transport, its efficacy is lower (~70%) as opposed to the Moderna and Pfizer/BioNTech vaccines, which have efficacies of 95% and 90%, respectively.2–4
All three vaccines require two doses at different intervals to achieve full efficacy.
With this in mind, the logistics of developing and distributing an effective vaccine to the world’s population of almost eight billion people is set to provide some issues.
Here, Nigel Theobald, CEO, N4 Pharma, looks at the vaccine race and the hurdles that could be overcome by using a silica nanoparticle delivery system.
Which systems are showing best results?
As of 5 January 2021, there were 73 vaccine candidates in development and more than 192 trials and seven approved vaccines globally. Of those, the two approved vaccines with the highest level of efficacy — from Pfizer/BioNTech and Moderna — both use nucleic acids (specifically messenger RNA).5

Nigel Theobald, CEO, N4 Pharma
Although these novel vaccines clearly highlight the huge potential for nucleic acid-based vaccines, there are challenges in their delivery, such as the storage conditions required for distribution, scale-up for mass production and cost of production and rollout.
The characteristics of a good vaccine delivery system include high loading capacity, controlled release with an extended half-life, no leakage and no interference with the stability of the therapeutic module.
Delivery systems should also offer a straightforward/consistent manufacturing process (particularly in the case of COVID-19, wherein time is of the essence), good biocompatibility, low toxicity, biodegradability and a clear mode of action.
Lipid nanoparticles
The Moderna and Pfizer (with BioNTech) vaccines use mRNA for speed of production.
These vaccines target the “spike” protein of the virus, which is expressed on the surface and allows the virus to bind to the ACE2 receptor on the cell’s surface, initiating the uptake by the cell and replicating the virus to trigger an immune response.
However, one of the biggest difficulties with DNA/RNA vaccines is getting the host cell to accept the genetic material. The two most common methods for this use viral vectors or a delivery system to carry the DNA/RNA across the cell membrane.
To get the mRNA strand inside a cell, scientists encase it in a lipid nanoparticle, which has inherent limitations. Lipids are sensitive to heat and will stop working if they exceed a certain temperature, hence the requirement for the two mRNA vaccines to be kept at very low temperatures.
Other disadvantages of lipids include cell toxicity, the release of systemic inflammatory cytokines, possible accumulation in the liver and spleen (with the resulting possibility of hepatotoxicity), low drug payloads for hydrophilic molecules and the potential of the reticuloendothelial system (RES) to act as a major route of clearance if liposomes are administered systemically.
The challenge is to deliver enough nucleic acid into the cells without unwanted side-effects.
Adenovirus-based
In the UK, Oxford University’s vaccine (in collaboration with AstraZeneca) began rollout in January 2021, albeit with lower vaccine efficacy (70%) than the two mRNA vaccines.
This vaccine uses ChAdOx1 nCoV-19, a weakened version of a common cold virus that causes infection in chimpanzees.6
Viral vectors such as this are favoured in the development of COVID-19 vaccines for effective delivery because they are able to replicate the spike protein from SARS-CoV-2 and resemble a natural infection, triggering an immune response.
However, producing the viral vectors can be a challenging process and, thus, any improvement to that process could result in more vaccines being available faster.
The viral vector-producing cells need to be transfected with multiple plasmids carrying various viral genes and the payload (the vaccine). This may make it difficult to scale-up, particularly to the volume required for global vaccination programmes.
Electroporation
Other nucleic acid candidates for a COVID-19 vaccine use DNA rather than mRNA, such as that being developed by Inovio.
These typically use electroporation as the delivery method whereby a high-voltage electrical current is applied to a living cell, which makes it temporarily permeable and allows a foreign material, such as DNA, to pass through.
However, it causes pain and discomfort at the site of injection compared with conventional vaccine delivery systems … among other drawbacks. This method requires specialist equipment, plus training medical staff in administering the vaccine and is very expensive, which will be a significant barrier to its widespread adoption.
A new contender
Silica nanoparticles, although not a silver bullet, offer promise as a delivery system that could overcome many of the issues currently being raised as barriers to an effective COVID-19 vaccination programme.
Silica is “Generally Recognized As Safe” by the United States Food and Drug Administration (FDA) and has been proven in recent years in various biomedical applications.
Mesoporous silica nanoparticles (MSNs) — silica-based nanostructured materials with strong biocompatibility and chemical stability — are a suitable candidate for vaccine delivery. Nanoparticulate silica can also be re-engineered to bind oligonucleotides of varying sizes, including DNA, RNA and SiRNA.
Nuvec’s role
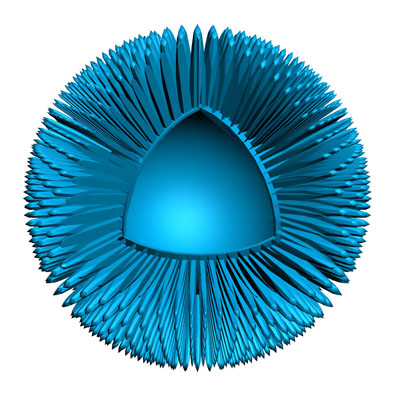
N4 Pharma’s novel silica nanoparticle, Nuvec, is specifically designed for nucleic acid delivery. It has an irregular (spiky) surface structure, functionalised by coupling with polyethyleneimine (PEI).
This surface simply and effectively traps and protects nucleic acids (such as mRNA/pDNA) as it travels to the cells. The Nuvec particle carrying the DNA/RNA attaches to the cell membrane and is taken up into the cell via general and dynamic endocytosis.
Once inside, PEI changes its charge and begins to disassociate from the particle, releasing some DNA/RNA. The particle spikes then start to disintegrate, releasing more of the nucleic acid into the endosome.
The released PEI ruptures the endosome membrane, releasing the DNA/RNA into the cytoplasm. It is then free to be taken up into the nucleus where it expresses protein, which is presented on the cell membrane to attract and activate T-cells.
Nuvec is also a natural adjuvant, so it attracts many innate immune cells which, in turn, leads to further activation of the adaptive immune system (T and B cells). It has also been shown to generate strong interferon gamma production (TH1 response).
Advantages compared with other delivery systems
Nuvec as a nucleic acid delivery system has already shown that it does not exhibit any unwanted systemic side-effects. Data reveals that the trapped drug remains at the site of injection, does not produce unwanted inflammatory responses and, most importantly, does not track to the liver.
A series of studies has supported the safety, efficacy and mode of action of Nuvec, and N4 Pharma is currently conducting preclinical COVID-19 proof of concept research using a DNA plasmid encoded for the SARS-CoV-2 spike protein.
It was confirmed in August 2020 that Nuvec loaded with a coronavirus plasmid successfully transfected Human Embryonic Kidney (HEK) cells in vitro and induced expression of the spike protein in the cells. N4 Pharma is now undertaking in vivo studies to demonstrate the capability of Nuvec to generate COVID-19 specific antibodies.
Crucially, Nuvec can be formulated with plasmid DNA, dried and stored at room temperature or in the fridge at 4 °C for at least 14 days (with further work under way to test longer time periods), then reconstituted without any degradation of DNA — all while maintaining good transfection.
This is important because a stable, easy to store and use vaccine is a major challenge for developers.
Next steps
The race to develop a COVID-19 vaccine has been won by nucleic acid-based vaccines; but, the future of development for COVID-19 vaccines is far from complete.
As well as the absolute vaccine efficacy, we must also consider the safety, ease of use and transportation to determine which of the vaccines can be widely distributed across populations.
Otherwise, effective immunity is going to be extremely unlikely. It is also expected that the COVID-19 virus will continue to mutate and future vaccines may well need to be adapted and reformulated, possibly on an annual basis like the influenza vaccine.
Having a vaccine that can be easily stored and distributed is important; sufficient numbers must be vaccinated each year for regular effective immunity to be achieved in a large enough proportion of the population.
Established delivery systems such as lipid nanoparticles or electroporation both have serious limitations in terms of storage and mass-scale distribution.
References
- www.biopharmadive.com/news/moderna-pfizer-biontech-coronavirus-vaccine-stability/584209.
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/950250/Information_for_UK_healthcare_professionals_on_COVID-19_Vaccine_AstraZeneca.pdf.
- https://doi.org/10.1136/bmj.m4471.
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/948517/Information_for_Healthcare_Professionals_on_Pfizer_BioNTech.pdf.
- https://covid19.trackvaccines.org/vaccines.
- www.research.ox.ac.uk/Article/2020-07-19-the-oxford-covid-19-vaccine.
